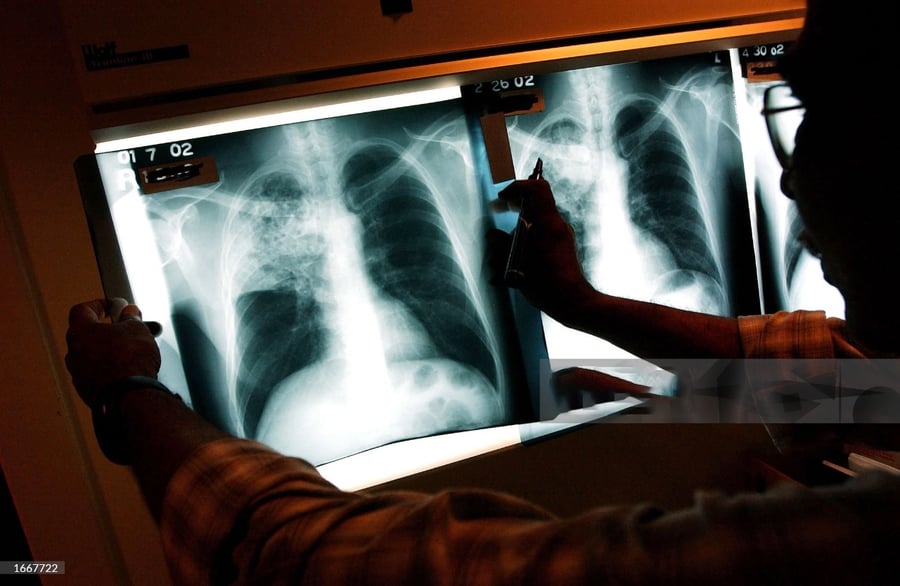
Tuberculosis Surgery in Dubai
The tuberculosis bacterium is known to require oxygen for survival. In the past, medical professionals believed that by blocking the entry of oxygen into the cavities, it would be beneficial for patients with cavitary pulmonary tuberculosis.
Historically, the treatment for tuberculosis involved a technique called collapse therapy. This involved various methods such as thoracoplasty, wax or lucite ball plombage, phrenic nerve crush or interruption, pneumoperitoneum, and induced pneumothorax.
Collapse therapy remained the preferred treatment option for tuberculosis infections until the introduction of chemotherapy with streptomycin and para-aminosalicylic acid (PAS) in 1945. However, it wasn't until the discovery of isoniazid in 1952 that prolonged cures could be achieved through antibiotic therapy.
Over time, resectional surgery gradually replaced collapse therapy as the primary surgical approach for patients with tuberculosis infections and severely damaged lungs or cavitary disease. The introduction of rifampin in 1966 significantly reduced the need for surgery, and the sanatoria system eventually became obsolete.
In most cases, drug-sensitive tuberculosis can be successfully treated with antibiotic therapy alone. The standard treatment for drug-sensitive tuberculosis typically involves a combination of INH, rifampin, and a short course of pyrazinamide.
Patients with drug-sensitive tuberculosis undergo surgery only in cases of complications, including the need to rule out cancer, experiencing massive hemoptysis (coughing up more than 600 cc of blood in 24 hours), dealing with bronchostenosis or bronchoectasis, or requiring decortication of a trapped lung. This occurs when there is polymicrobial contamination within the pleural cavity in tuberculosis patients who have previously had a pleural effusion.
Patients who have tuberculosis and are resistant to both INH and rifampin are categorized as having multidrug-resistant tuberculosis (MDRTB), which poses a significant challenge for surgeons. These patients often exhibit resistance to the three other first-line drugs, including ethambutol, streptomycin, and pyrazinamide, and may also be resistant to several second-line drugs.
MDR-TB patients undergo surgery for various reasons, as mentioned earlier, including persistent cavitary disease with or without a positive sputum, as well as a destroyed lobe or lung with or without a positive sputum. Remarkably, MDR-TB patients represent the largest group of individuals who require surgery for pulmonary tuberculosis infections.
Preparation for surgery
Preparation for surgery plays a crucial role in the treatment of patients with mycobacterial infections. One key aspect of this preparation is ensuring proper nutrition. Patients with albumin levels below 3.0 g/dl are not eligible for surgery. To improve their overall health before the procedure, nutritional supplementation can be administered orally or through gastrostomy or jejunostomy feeding tubes. Additionally, the best available antibiotic therapy is given for approximately three months leading up to the surgery. It's important to note that in cases of multidrug-resistant tuberculosis (MDR-TB), only about half of the patients have negative sputum prior to surgery.
As part of the routine evaluation, pulmonary function tests, ventilation-perfusion scans, and computed tomography are conducted, similar to other pulmonary surgeries.
Surgical principles include:
- During the surgical procedure, it is essential to preserve enough healthy lung tissue to ensure a successful recovery for the patient. Our experienced surgeons utilize double-lumen tubes or bronchial blockers in all operations to optimize the surgical outcome. While removing any grossly affected lung tissue, including cavitary disease and severely damaged areas, we aim to preserve any nodular disease present in other parts of the lung.
- To minimize fluid administration during surgery, we strive to keep it below 1200 cc whenever possible, and for pneumonectomies, below 800 cc.
- Muscle flaps, such as the latissimus dorsi muscle and intercostal muscle, play a vital role in reducing bronchopleural fistula and filling empty spaces during certain cases, including pneumonectomy, polymicrobial contamination, and positive sputum at the time of surgery. On the other hand, omental flaps are utilized in situations involving massive contamination, previous surgery, and other specific circumstances.
In cases of extensive contamination, the chest is deliberately left open using the Eloesser procedure. It is then packed with Kerlix gauze soaked in a half-strength Dakin's solution, and this dressing is changed daily for a period of 5 to 6 weeks. Once the contamination is under control and the intrathoracic chest wall is deemed clean, Clagett's solution is left in the pleural cavity before closing the chest.
While the use of pleural tents has been suggested to help seal air leaks and eliminate space, they are not practical in mycobacterial surgery due to the specific dissections performed over the upper lobe in the extra pleural plane.
Postoperatively, appropriate antibiotic therapy is continued to ensure a successful recovery. It is important to note that in experienced hands, the operative mortality rate should be less than 5%, highlighting the expertise and skill of the surgical team.
Complications
- Complications can occur in approximately 25-30% of cases, but with the expertise and experience of our surgical team, we are able to reduce this rate to less than 15%. One common complication is bronchopleural fistula, which tends to occur more frequently after right pneumonectomy, with a rate of around 20% in cases without the use of muscle or omental buttress. Wound infections and abscesses are also common complications that can arise. Additionally, there may be concerns related to the apical space. Other potential complications, such as air leaks, bleeding, and postpneumonectomy pulmonary edema, are similar to those encountered in other thoracic procedures for non-mycobacterial diseases.
- For top-notch thoracic surgery in Dubai, contact DRHC at +97142798200. We offer expert thoracic surgeons and comprehensive care.