Paracentesis / Abdominal Tapping in Dubai at DRHC
Introduction:
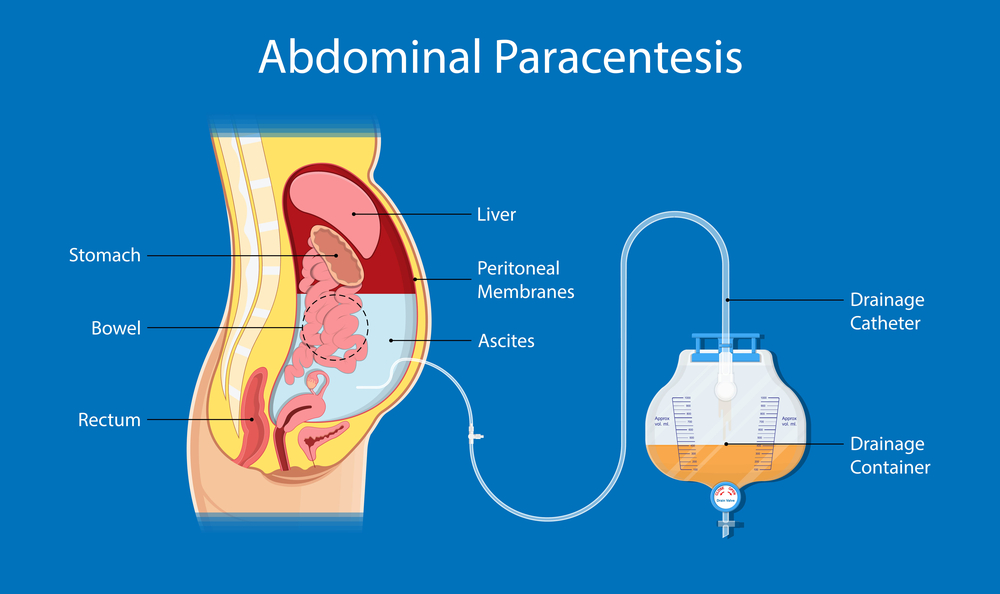
Paracentesis is the procedure by which we remove fluid from the peritoneal cavity. It is called diagnostic paracentesis (when done to search for the etiology, a milliliter) and therapeutic (when to evacuate five liters or more for symptomatic relief). It is a simple bedside procedure to relieve the associated dyspnea, abdominal pain, and early satiety.
Indications:
It is performed safely by a doctor who has undergone the necessary training. The purpose is to diagnose and manage the situation appropriately (for instance, the type of bacteria and their susceptibility to a specific antibiotic)
It's done for the following reasons:
- New-onset ascites
- Hospitalization of a patient with ascites
- Tense ascites management (diuretic-resistant, dyspnea, and inability to eat)
- Clinical deterioration of a previously stable situation (Fever, Abdominal pain, Hepatic encephalopathy, Peripheral leukocytosis, Deterioration in renal function, and Acidosis)
Despite being relatively safe, patients with abnormal coagulation tests and thrombocytopenia must be used cautiously. (There is no evidence to support coagulation testing before paracentesis at this point.)
The Technique:
The purpose of paracentesis is to have a good and clean sample of the fluid to study or remove. Proper technique is important to decrease the risk of sample contamination and complications.
Our Step-By-Step Approach:
- Preparation of blood culture bottles and sturdy tubes with the needed material ahead
- Positioning the Patient (supine, flat, or slight head elevation)
- The needle entry site (through the left lower quadrant abdominal wall). In the midline cephalad or caudad to the umbilicus, surgical scars and abdominal wall collateral vessels may be present, and they should be avoided.
- In practice, the "left McBrney's" localization (McBurney's point is one-third of the distance from the left anterior superior iliac spine to the umbilicus) requires dullness to percussion, the absence of the spleen, and the absence of surgical scars within a few centimeters of the intended entry site. If there is any doubt, an ultrasound can be used to confirm the presence of fluid as well as the absence of the bowel or spleen within the needle range.
- We use iodine or chlorhexidine to sterilize the skin at and around the chosen spot. Nonsterile gloves are used for sterilization. If the fluid has dried by the time the skin is contacted, sterility is improved. Anesthetizing the site of puncture. After that, the doctor puts on sterile gloves and draws a 1% lidocaine solution into a sterile 3 to 5 mL syringe.
- We must try to reach the fluid with the anesthetic syringe and needle to confirm the presence of fluid and the depth of penetration needed to reach the ascites.
- The paracentesis needle should be placed into the anesthetized route.
- Once the paracentesis needle has entered the peritoneal cavity and fluid is aspirated, the needle must be stabilized so that it does not pull out of the peritoneal cavity.
- When there isn't much fluid present, obtaining a free flow of fluid might be challenging. This is because the bowel or omentum may block the end of the needle. Multiple-hole needles (primarily used for therapeutic paracentesis) help avoid this problem because fluid can still enter the needle through the side holes even if the end hole is blocked.
- Ascitic fluid can be collected for diagnostic testing once it has started to flow.
- Removing large volumes of fluid (therapeutic paracentesis) — A large-volume paracentesis is described as the removal of more than 5 liters of ascitic fluid. To make a patient comfortable, patients with tight ascites should have enough fluid removed to relieve intra-abdominal pressure. To minimize the amount of fluid, a sodium-restricted diet and diuretics are employed.
- The colon and omentum are more likely to occlude the needle hole(s) when the fluid level drops, slowing or stopping the flow of fluid. If the flow slows, we can slowly and gently shift the patient's position to reposition the fluid. The longer the delay between procedures, the more fluid is evacuated with each paracentesis. (caution due to the patient's underlying medical condition)
The catheter is then removed at the end of the treatment, and the patient can be discharged home after 30-60 minutes of observation. After a few days, the liquid's laboratory results will be available.
.png?width=281&height=59&name=bookanappointment%20(1).png)
If you are due for a Paracentesis / Abdominal Tapping or are experiencing gastrointestinal symptoms, don't delay. Contact DRHC Dubai to schedule your appointment. Our team of experts is here to provide you with compassionate care and personalized treatment to keep your digestive health in check. To book Your Appointment, just call us at +97142798200 for a consultation with the Gastroenterology Clinic at DRHC Dubai.


%20(1).png)
.png?width=281&height=59&name=bookanappointment%20(1).png)




