Thyroid Anatomy at DRHC Dubai
Dr. Rami Hamed Center in DHCC provides thyroid surgery in Dubai with the leading thyroid specialist in Dubai for complete care of thyroid diseases, including all diagnostic modalities and the latest nonsurgical and surgical techniques available for the best outcomes.
Thyroid Anatomy:
We should know thyroid anatomy to avoid thyroid surgery and any complications that may arise after the surgery.
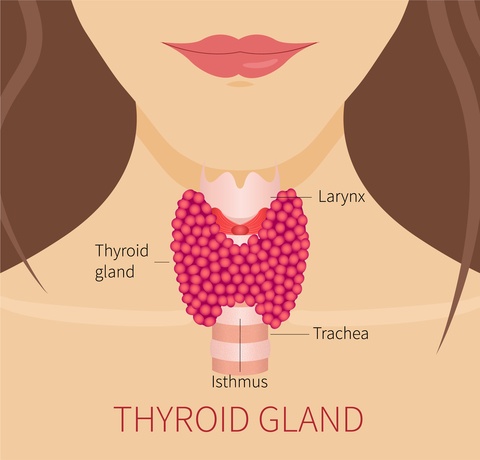
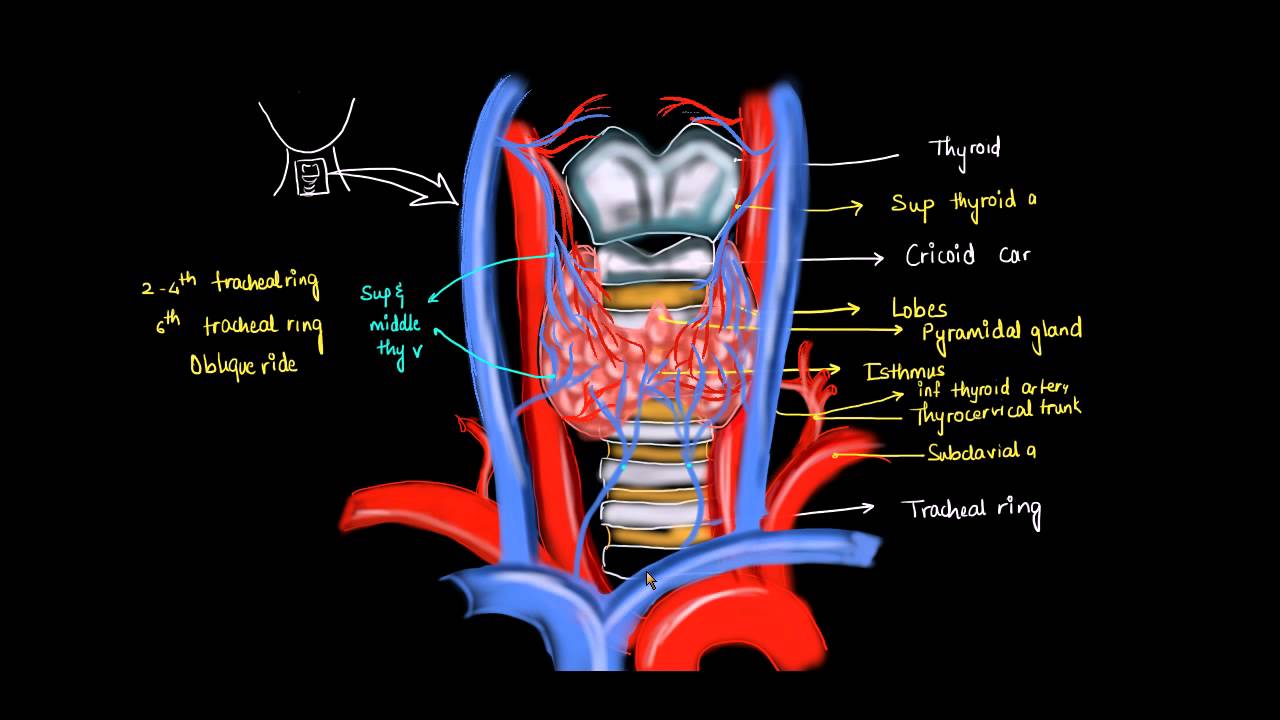
The anatomical relationships of the thyroid gland and surrounding structures are depicted in the picture. The adult thyroid gland is brown in color and firm in consistency and is located posterior to the strap muscles. The normal thyroid gland weighs approximately 20g. The thyroid lobes are located adjacent to the thyroid cartilage and connected in the midline by an isthmus. A pyramidal lobe is present in about 50% of patients. The strap muscles are located anteriorly and are innervated by the ansa cervicalis. The thyroid gland is covered by a loose fascia, the true capsule, which is a thin, densely adherent fibrous layer that sends out septa-forming pseudolobules. The thyroid capsule becomes Berry's ligament near the cricoid cartilage and upper tracheal rings.
The superior thyroid arteries:
branches from the external carotid arteries divide into anterior and posterior
The inferior thyroid arteries:
These arise from the thyrocervical trunk shortly after their origin from the subclavian arteries. The inferior thyroid arteries travel upward in the neck posterior to the carotid sheath to enter the thyroid lobes at their midpoint.
A thyroid ima artery:
It arises directly from the aorta or innominates in 1 to 4% of individuals to enter the isthmus or replace a missing inferior thyroid artery. The inferior thyroid artery crosses the recurrent laryngeal nerve (RLN), necessitating identification of the RLN before the arterial branches can be ligated. The venous drainage of the thyroid gland occurs via multiple small surface veins, which coalesce to form three sets of veins—the superior, middle, and inferior thyroid veins. The superior thyroid veins run with the superior thyroid arteries bilaterally. The middle vein or veins are the least consistent. The superior and middle veins drain directly into the internal jugular veins. The inferior veins drain into the brachiocephalic veins.
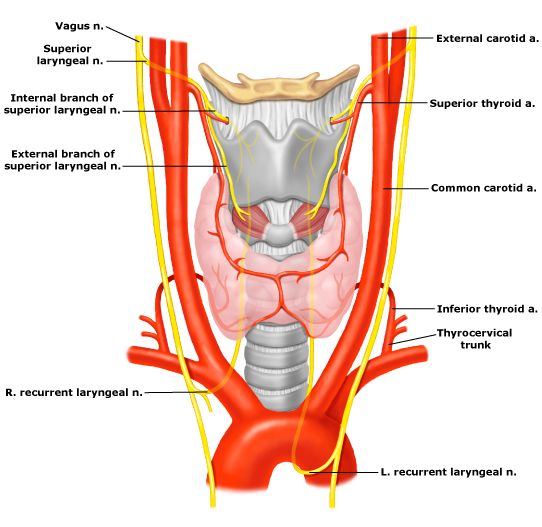
Thyroid Nerves:
The left recurrent laryngeal nerve (LRLN) arises from the vagus nerve, where it crosses the aortic arch, loops, and ascends directly in the neck within the tracheoesophageal groove. The right RLN arises from the vagus at its crossing with the right subclavian artery. The nerve usually passes posteriorly to the artery before ascending in the neck. It's, of course, more oblique than the left RLN. Along their course in the neck, the RLNs may branch and pass anterior, posterior, or interdigitate with branches of the inferior thyroid artery.
RLNs are rare but have been reported in patients with situs inversus and a right-sided aortic arch. The RLNs innervate all the intrinsic muscles of the larynx, except the cricothyroid muscles, which are innervated by the external laryngeal nerves. Injury to one RLN leads to paralysis of the ipsilateral vocal cord, which comes to lie in the paramedian or abducted position. The abducted position leads to a hoarse voice and an ineffective cough.
A bilateral RLN injury may lead to airway obstruction, an ineffective cough, and aspiration necessitating an emergency tracheostomy. The superior laryngeal nerves also arise from the vagus nerves. After their origin at the base of the skull, they divide into two branches at the level of the hyoid bone. The internal branch of the superior laryngeal nerve is sensory to the supraglottic larynx. Injury to this nerve is rare in thyroid surgery, but its occurrence may result in aspiration. The external branch of the superior laryngeal nerve lies on the inferior pharyngeal constrictor muscle and descends alongside the superior thyroid vessels before innervating the cricothyroid muscle relationship of this nerve to the superior thyroid vessels.
Sympathetic innervation
The thyroid gland is provided by fibers from the superior and middle cervical sympathetic ganglia. The fibers enter the gland with the blood vessels and are vasomotor in action.
Parasympathetic:
Fibers are derived from the vagus nerve and reach the gland via branches of the laryngeal nerves.
Thyroid Lymphatic System:
It is important to understand the lymphatic system of the thyroid to understand how thyroid cancer is spread. The thyroid gland is an extensive network of lymphatics. Intraglandular lymphatic vessels connect both thyroid lobes through the isthmus and also drain to peri-thyroidal structures and lymph nodes. Regional lymph nodes include paratracheal, RLN, superior mediastinal, paratracheal, peri-thyroidal, retropharyngeal, esophageal, and upper, middle, and lower jugular chain nodes.
.png?width=281&height=59&name=bookanappointment%20(1).png)
Dubai Thyroid Clinic: DRHC provides the best thyroid surgeon in Dubai and treatment for hypothyroidism, hyperthyroidism, thyroid cancer, thyroid disease, thyroidectomy, and thyroid surgery. DRHC provides advanced thyroid tests in Dubai. To book your Appointment please call +97142798200.



.png?width=281&height=59&name=bookanappointment%20(1).png)
.webp?width=1080&height=1080&name=Doctor%20background%20For%20Website%20Dr.%20Fadi%20Nageeb%2009%20(1).webp)
.webp?width=1080&height=1080&name=Doctor%20background%20For%20Website%20Dr%20Abdul%20Majeed%20Khalid%20%2002%20(1).webp)



