Lumbar Disc Prolapse - Spine Hospital DRHC Dubai
Which Lumbar Disc prolapse do we treat surgically?
In the first three months of onset, we operate on disc prolapses causing severe uncontrollable pain (Sciatica) and/or associated with neurological deficit, and of course, in cases of huge prolapses with impending features of ‘Cauda Equina’ syndrome. Call +97142798200 and get the best back pain treatment in Dubai.
After the first three months, we operate, in addition to the above, on cases with pain interfering significantly with lifestyle and not settling on conservative treatment.
Conservative treatment of Lumbar disc prolapse:
Conservative management is indicated in the absence of neurological deficits and in certain cases associated with co-morbidity. The old-fashioned treatment of bed rest, wooden board, floor bed, etc, is ineffective and out of question.
- Pain control: Usually by using balanced analgesia techniques, which means using different painkillers with different mechanisms of action, including simple painkillers, non-steroidal anti-inflammatories, morphine, etc.
- Muscle relaxants: Used to alleviate the vicious circle of pain and spasm, and facilitate active physical therapy and rehabilitation, I am a great fan of Valium as a muscle relaxant, as it makes wonders with patients with acute pain.
- Physiotherapy and Lumbar disc prolapse: physiotherapy's role is to facilitate the return to usual activities and safely mobilize the spine. It may include manual techniques, dry needling, and traction depending on the case. In the market, there are advocates for special traction devices and magnetic devices. We do not support these methods as it is not supported by any objective research, and we consider them ineffective without any randomized controlled trial. Osteopaths and chiropractors' involvement is reasonable, but they do not have magic hands when compared to physiotherapists. Our physiotherapists specialize in disc prolapse physiotherapy.
- Epidural injection: Epidural injection is a great, simple, and safe method to treat lumbar disc prolapses with a 50% chance of success. Its mechanism of action is to reduce pain to a tolerable limit and reduce the inflammation around the nerves in the spinal canal. It can be repeated up to three times and can simply cure you.
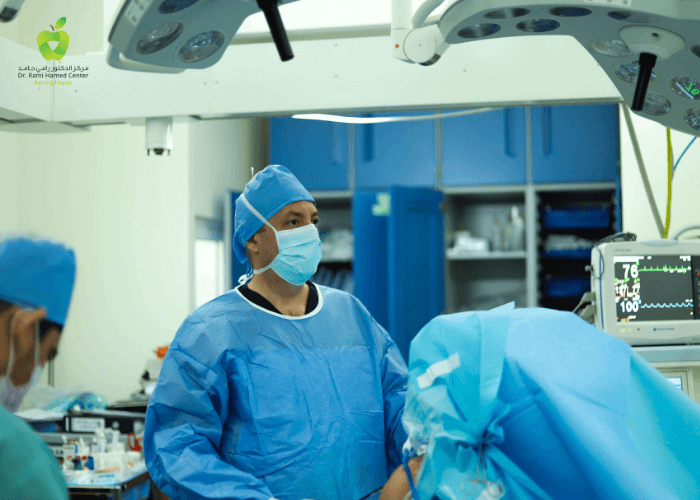
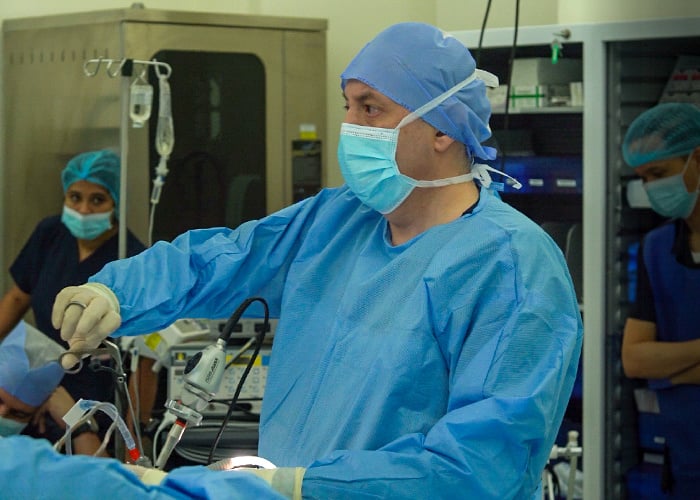
Surgical treatment of Lumbar disc prolapse:
The cases estimated to require surgery are only 7% of the total cases, in which conservative treatment failed, and in the presence of a neurological deficit. There are many techniques for lumbar discectomy surgery. All techniques share the same philosophy of removing the pressure on the nerves without damaging the spine and the surrounding soft tissue. Patient selection, surgeon preference, and advanced instrument availability are the keys to a successful outcome. Surgery for prolapse at DRHC has a huge record of success. DRHC offers the best herniated disc treatment in Dubai.
In this respect, I will explain some of the available techniques and their advantages and disadvantages for public understanding.
Laser Discectomy:
There is a thing called Laser Discectomy in spinal surgery; some surgeons use laser probes and coagulate the disc space after finishing the microdiscectomy procedure, but this has no scientifically proven advantage, and it is possibly used or designed for marketing and propaganda purposes.
Complications of Lumbar Micro Discectomy:
The complication risk is 2-3%; complications are usually minor and reversible, including minor weakness, sensory disturbance, hemorrhage, infection, Dural tear, and CSF leak. The major complications of paralysis and inability to function, including Cauda Equina syndrome, are theoretical in our current era and experienced hands.
Please follow the links below to read more about the various techniques.
Read our Blogs:




.png?width=281&height=59&name=bookanappointment%20(1).png)